Introduction to Psychotic Disorders
Psychotic disorders Symptoms Causes and Treatment are often misunderstood, feared, and surrounded by stigma. When people hear the word psychosis, they imagine something extreme or dangerous. In reality, psychotic disorders are complex mental health conditions that affect how a person thinks, feels, and understands reality. They are medical conditions, not character flaws.
Understanding psychotic disorders is the first step toward compassion, early treatment, and recovery. Let’s break it all down in simple, human language.
What Are Psychotic Disorders?
Psychotic disorders are mental health conditions in which a person loses touch with reality. This may involve seeing or hearing things that aren’t there, believing things that are not true, or thinking in ways that don’t make sense to others.
Think of the mind like a radio. In psychosis, the signal gets distorted. The brain misinterprets information, making reality feel confusing or even frightening.
Why Understanding Psychosis Matters
Psychosis can affect anyone, regardless of age, gender, or background. Early understanding leads to early help, and early help can change lives. When ignored, symptoms can worsen, affecting relationships, work, education, and overall quality of life.
Understanding Psychosis

What Is Psychosis?
Psychosis is not a diagnosis on its own. It’s a symptom or a group of symptoms that appear in several mental health disorders. During psychosis, a person may struggle to distinguish between what’s real and what’s not.
Psychosis vs. Reality
Imagine dreaming while awake. That’s often how people describe psychosis. Hallucinations feel real. Delusions feel logical. The experience is genuine to the person, even if it doesn’t align with reality.
Common Misconceptions About Psychosis
Many believe psychosis means violence or “madness.” That’s simply not true. Most people with psychotic disorders are not dangerous. In fact, they are more likely to harm themselves than others due to fear and confusion.
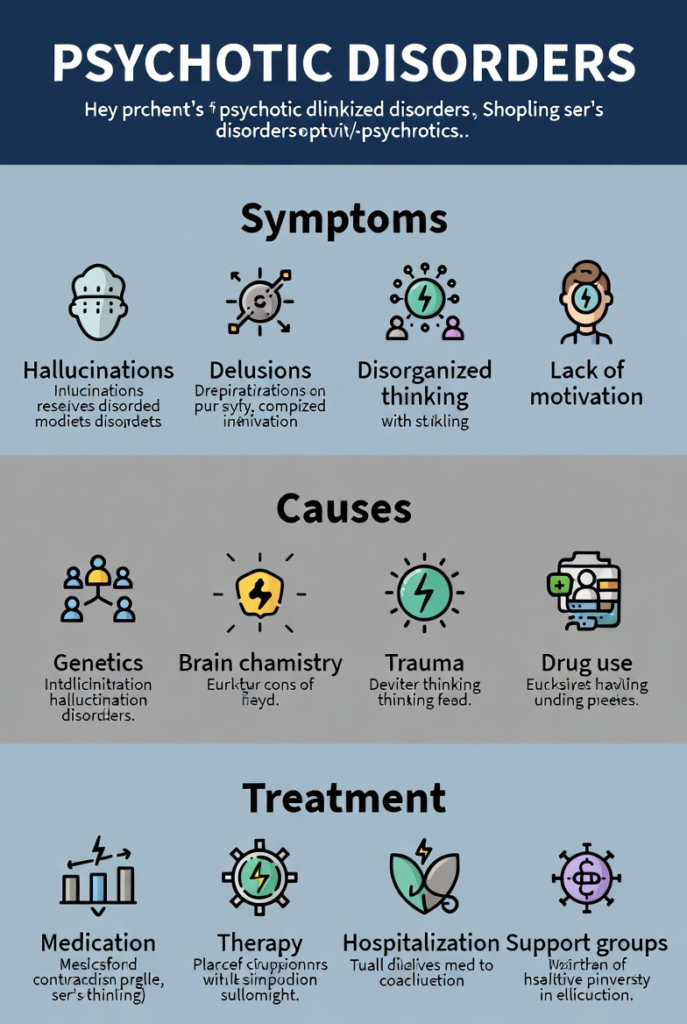
Types of Psychotic Disorders
Schizophrenia
Schizophrenia is one of the most well-known psychotic disorders. It involves long-term symptoms like hallucinations, delusions, disorganized speech, and reduced emotional expression. It usually begins in late adolescence or early adulthood.
Schizoaffective Disorder
This condition combines symptoms of schizophrenia with mood disorder symptoms, such as depression or bipolar disorder. A person may experience psychosis alongside intense mood swings.
Delusional Disorder
In delusional disorder, the main symptom is one or more strong delusions that last for at least a month. Unlike schizophrenia, daily functioning may remain mostly intact.
Brief Psychotic Disorder
This disorder involves sudden, short-term psychotic episodes often triggered by extreme stress or trauma. Symptoms usually last less than a month and may resolve completely.
Substance-Induced Psychotic Disorder
Alcohol, drugs, or medications can trigger psychosis. Substances like cannabis, amphetamines, and hallucinogens are common triggers, especially with heavy or long-term use.
Psychotic Disorder Due to Medical Conditions
Certain medical conditions, such as brain injuries, epilepsy, infections, or autoimmune diseases, can cause psychotic symptoms.
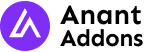
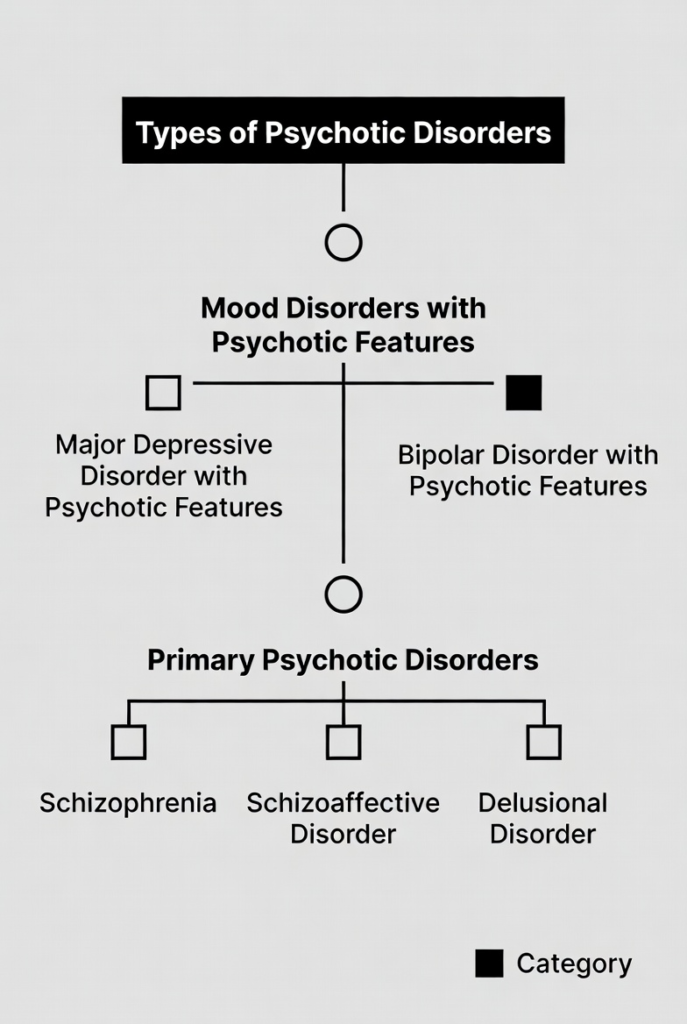
Core Symptoms of Psychotic Disorders
Positive Symptoms
Positive symptoms add something unusual to a person’s experience.
Hallucinations
Hallucinations involve seeing, hearing, smelling, tasting, or feeling things that aren’t there. Hearing voices is the most common type.
Delusions
Delusions are strong beliefs that persist despite clear evidence against them. These may include paranoia, grandiosity, or false beliefs about being controlled.
Negative Symptoms
Negative symptoms remove or reduce normal functioning.
Emotional Flatness
People may show little emotion, speak less, or appear disconnected.
Social Withdrawal
Loss of interest in social activities, relationships, or daily routines is common.
Cognitive Symptoms
These affect thinking abilities, such as poor concentration, memory problems, and difficulty making decisions.
Causes and Risk Factors
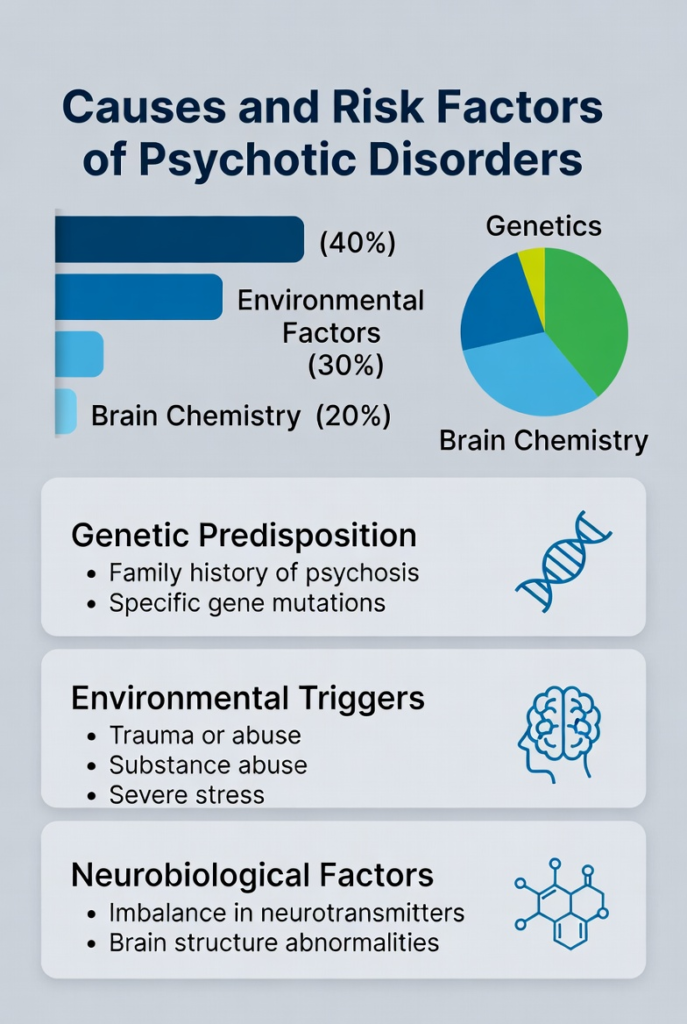
Biological Factors
Imbalances in brain chemicals like dopamine play a major role. Brain structure and function differences are also linked to psychosis.
Psychological Factors
Trauma, chronic stress, and childhood abuse can increase the risk of psychotic disorders.
Environmental and Social Factors
Urban living, social isolation, poverty, and substance abuse are associated with higher risk.
Genetic Vulnerability
Psychotic disorders often run in families. Having a close relative with schizophrenia increases risk, but genetics alone don’t determine outcomes.
Diagnosis of Psychotic Disorders
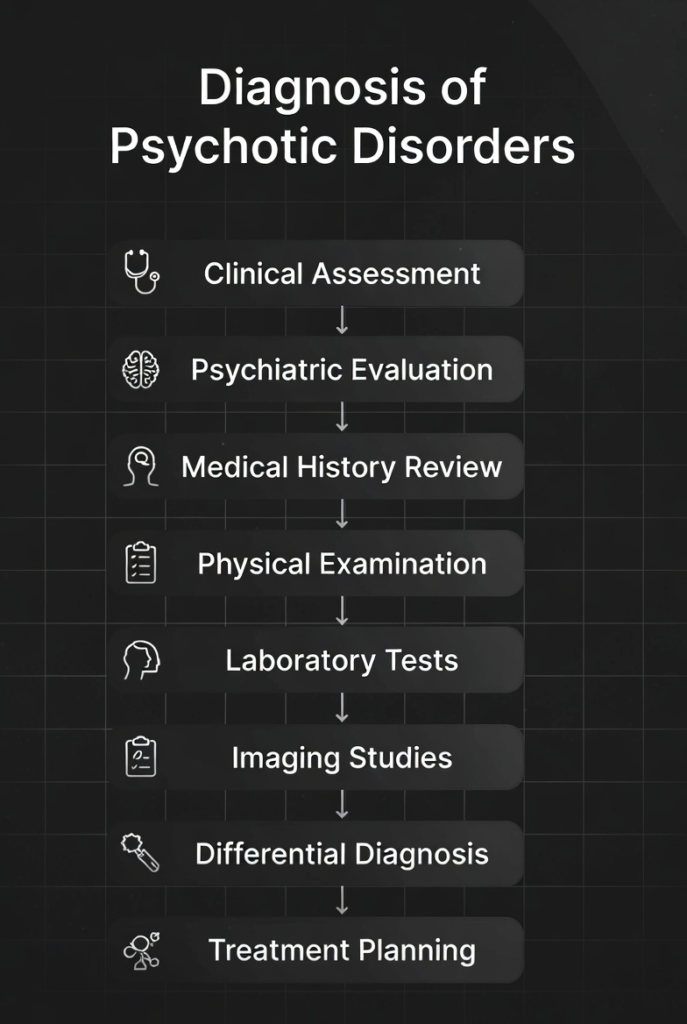
Clinical Assessment
Diagnosis involves detailed interviews, observation, and medical history review. Mental health professionals assess symptoms, duration, and impact.
Diagnostic Criteria
Clinicians use standardized guidelines to differentiate between types of psychotic disorders.
Challenges in Diagnosis
Symptoms may overlap with depression, bipolar disorder, or substance use, making diagnosis complex.
Treatment Options for Psychotic Disorders
Antipsychotic Medications
These medications help reduce hallucinations and delusions by balancing brain chemicals. Finding the right medication may take time.
Psychotherapy
Therapy helps individuals understand their experiences and cope with symptoms.
Cognitive Behavioral Therapy (CBT)
CBT helps challenge distorted thoughts and develop healthier thinking patterns.
Family Therapy
Educating families improves communication and reduces relapse risk.
Hospitalization and Crisis Care
In severe cases, short-term hospitalization ensures safety and stabilization.
Living With a Psychotic Disorder
Daily Life Challenges
Managing symptoms, medication side effects, and social stigma can be overwhelming.
Coping Strategies
Routine, stress management, therapy, and medication adherence play a key role.
Importance of Support Systems
Support from family, friends, and mental health professionals can make recovery possible.
Psychotic Disorders in Children and Adolescents
Early Warning Signs
Social withdrawal, odd behavior, academic decline, and unusual fears may appear early.
Impact on Development
Early-onset psychosis can affect emotional, social, and cognitive development if untreated.
Stigma and Psychotic Disorders
Social Stigma and Myths
Stigma leads to discrimination, silence, and delayed treatment.
Breaking the Silence
Education, open conversations, and empathy help reduce stigma and encourage help-seeking.
Recovery and Long-Term Outlook
Is Recovery Possible?
Yes. Many people manage symptoms effectively and lead meaningful lives with proper treatment.
Managing Relapses
Early warning signs, medication adherence, and stress reduction help prevent relapses.
Prevention and Early Intervention
Identifying Early Symptoms
Early intervention programs improve long-term outcomes significantly.
Role of Mental Health Awareness
Awareness reduces stigma and promotes timely treatment.
Additional Insights on Psychotic Disorders
Even after understanding symptoms and treatments, many readers still ask, “What does psychosis really look like in everyday life?” Let’s go a bit deeper and explore the human side of psychotic disorders—the parts that textbooks often miss.
Psychotic Disorders and Daily Functioning
Living with a psychotic disorder is not just about managing symptoms; it’s about navigating everyday life while carrying an invisible weight.
Simple tasks like going to work, studying, or maintaining relationships can feel overwhelming during active symptoms. Imagine trying to concentrate while your mind feels like a room full of overlapping conversations. That’s the reality for many people experiencing psychosis.
With proper treatment, structure, and patience, many individuals gradually rebuild routines and independence.
The Emotional Experience of Psychosis
Psychosis isn’t only confusing—it can be emotionally exhausting.
People often feel:
- Fear and anxiety due to hallucinations or paranoid thoughts
- Shame or embarrassment after episodes
- Frustration when others don’t understand their experiences
Emotional validation is crucial. Being told “it’s not real” can feel dismissive, even if well-intentioned. A more supportive approach is acknowledging the distress while gently guiding toward professional help.
Role of Family and Caregivers
Family members often feel helpless, confused, or even guilty. Supporting someone with a psychotic disorder requires patience and education.
Helpful actions include:
- Learning about the condition
- Encouraging treatment without force
- Avoiding arguments about delusions
- Offering calm reassurance
Families don’t need to have all the answers—just consistency and compassion.
Medication Myths and Facts
One common fear is that antipsychotic medications “change personality.” In reality, the goal is the opposite—to help the person reconnect with their true self.
Facts to know:
- Side effects vary from person to person
- Dosages can be adjusted
- Newer medications are generally better tolerated
- Stopping medication suddenly can increase relapse risk
Medication works best when combined with therapy and social support.
Psychosis and Substance Use
Substance use and psychosis often form a dangerous loop. Drugs may temporarily numb distress but can worsen symptoms long-term.
Substances commonly linked to psychosis include:
- Cannabis (especially high-potency strains)
- Amphetamines
- Cocaine
- Hallucinogens
Reducing or stopping substance use significantly improves treatment outcomes.
Hope, Identity, and Recovery
A diagnosis does not define a person. Many individuals with psychotic disorders:
- Finish education
- Maintain careers
- Build families
- Express creativity and purpose
Recovery is not about “never having symptoms again.” It’s about learning to live a fulfilling life despite challenges—like sailing with the wind instead of fighting the storm.
Final Reflection
Psychotic disorders remind us how delicate and powerful the human mind is. With knowledge, empathy, and proper care, fear turns into understanding and suffering turns into strength.
Conclusion
Psychotic disorders are serious but treatable mental health conditions. With early diagnosis, proper treatment, and strong support systems, individuals can regain control of their lives. Understanding psychosis replaces fear with empathy and silence with hope. Mental health matters—and so does compassion.
FAQs
1. Are psychotic disorders permanent?
Not always. Some people experience one episode, while others manage long-term symptoms with treatment.
2. Can stress cause psychosis?
Yes, extreme stress or trauma can trigger psychotic episodes, especially in vulnerable individuals.
3. Are people with psychosis dangerous?
No. Most are not dangerous and are more likely to be victims than perpetrators.
4. Can psychotic disorders be cured?
There is no single cure, but symptoms can be effectively managed with treatment.
5. When should someone seek help for psychosis?
Immediately, especially if hallucinations, delusions, or drastic behavior changes appear.
https://thewovenmind.com/wp-admin/post.php?post=320&action=edit