Anxiety disorders A Deep Dive Into the Mind’s Alarm System are more than just feeling nervous before a big presentation or uneasy during a turbulent flight. They are complex mental health conditions that quietly shape how millions of people experience the world every single day. Imagine having an internal alarm system that goes off not only when there’s real danger, but also when you’re simply checking your email, walking into a grocery store, or lying in bed at night trying to sleep. That’s what living with an anxiety disorder can feel like—exhausting, confusing, and often isolating.
In today’s fast-paced, always-connected world, anxiety disorders have become increasingly common. Deadlines pile up, social pressures intensify, and uncertainty seems to be everywhere. While stress is a normal part of life, anxiety disorders take that stress and amplify it, turning everyday situations into overwhelming challenges. What makes anxiety disorders especially tricky is that they’re often invisible. On the outside, someone might look calm and collected, while on the inside their mind is racing through worst-case scenarios at lightning speed.
This article takes a deep, human-centered look at anxiety disorders. We’ll unpack what they really are, why they happen, and how they show up differently from person to person. We’ll also explore treatment options, lifestyle changes, and practical strategies that actually help—not just in theory, but in real life. Whether you’re dealing with anxiety yourself, supporting someone who is, or simply want to understand the topic better, this guide is designed to feel like a conversation, not a textbook.
Anxiety disorders are not a personal weakness, a lack of willpower, or something you can simply “snap out of.” They are legitimate medical and psychological conditions, and the good news is that they are also highly treatable. Understanding them is the first step toward regaining a sense of control, calm, and confidence.
What Are Anxiety Disorders? Understanding the Basics

Anxiety disorders are a group of mental health conditions characterized by excessive fear, worry, or nervousness that interferes with daily life. Everyone experiences anxiety from time to time—it’s your brain’s way of keeping you alert and prepared. If a car suddenly swerves into your lane, anxiety helps you react quickly. If you have an important exam, anxiety might motivate you to study. In these cases, anxiety is helpful, even protective.
The problem begins when anxiety sticks around long after the threat is gone or shows up when there is no real danger at all. Anxiety disorders turn a helpful survival mechanism into a constant background noise that’s hard to turn off. The mind becomes stuck in “what if” mode, endlessly scanning for threats that may never come. What if I fail? What if I embarrass myself? What if something terrible happens?
One key difference between normal anxiety and an anxiety disorder is intensity and duration. Normal anxiety comes and goes. Anxiety disorders linger for weeks, months, or even years. They also tend to be disproportionate to the situation. A small mistake at work might feel like a career-ending catastrophe. A casual social interaction might feel like being under a spotlight with everyone judging your every move.
Anxiety disorders can affect how people think, feel, and behave. Emotionally, they can create a constant sense of dread. Physically, they can trigger symptoms like a racing heart, shortness of breath, muscle tension, and digestive issues. Behaviorally, they often lead to avoidance—skipping events, turning down opportunities, or isolating oneself to escape anxious feelings.
Understanding anxiety disorders starts with recognizing that they are not “just stress.” They involve complex interactions between brain chemistry, learned behaviors, genetics, and life experiences. Once you see anxiety disorders through this lens, it becomes clear why simple advice like “just relax” or “stop overthinking” misses the mark entirely.
The Science Behind Anxiety Disorders
To really understand anxiety disorders, it helps to peek under the hood and look at what’s happening inside the brain. Anxiety is deeply rooted in our biology. At the center of it all is the brain’s fear circuitry, particularly a small almond-shaped structure called the amygdala. The amygdala acts like a smoke detector, constantly scanning for danger. When it senses a threat—real or perceived—it sends out an alarm.
In people with anxiety disorders, this alarm system tends to be hypersensitive. The amygdala fires more easily and more often, even in situations that are objectively safe. Once the alarm is triggered, the body releases stress hormones like adrenaline and cortisol. These chemicals prepare you for “fight or flight” by increasing heart rate, sharpening focus, and redirecting energy to your muscles. That’s great if you’re escaping a predator, but not so helpful when you’re trying to sit through a meeting or fall asleep.
Neurotransmitters also play a major role. Chemicals like serotonin, dopamine, gamma-aminobutyric acid (GABA), and norepinephrine help regulate mood and anxiety levels. Imbalances in these neurotransmitters can make it harder for the brain to calm itself down after stress. This is one reason medications that target these chemicals can be effective for treating anxiety disorders.
Genetics add another layer to the puzzle. Research shows that anxiety disorders tend to run in families. This doesn’t mean anxiety is inevitable if a parent has it, but it does suggest a genetic vulnerability. Environmental factors—such as childhood experiences, trauma, chronic stress, or learned coping patterns—often determine whether that vulnerability turns into a full-blown disorder.
When you combine a sensitive fear system, chemical imbalances, and life experiences that reinforce worry or avoidance, anxiety disorders begin to make sense. They’re not random, and they’re not a flaw in character. They’re the result of a brain doing its best to protect you, just a little too aggressively.
Common Types of Anxiety Disorders

Anxiety disorders are not one-size-fits-all. They come in several distinct forms, each with its own patterns, triggers, and challenges. Understanding the different types can make it easier to recognize what you or someone else might be experiencing.
One of the most common types is Generalized Anxiety Disorder (GAD). People with GAD experience persistent, excessive worry about a wide range of everyday issues, such as work, health, money, or family. The worry feels difficult to control and often comes with physical symptoms like fatigue, muscle tension, and difficulty concentrating. It’s like having a mind that constantly expects something to go wrong.
Panic Disorder is marked by recurrent panic attacks—sudden surges of intense fear that peak within minutes. These attacks often come with physical sensations such as chest pain, shortness of breath, dizziness, and a feeling of losing control or dying. Because panic attacks are so frightening, many people develop a fear of having another one, which can lead to avoidance behaviors and even agoraphobia.
Social Anxiety Disorder revolves around a deep fear of social situations where one might be judged, embarrassed, or rejected. This goes beyond shyness. It can make everyday interactions—like speaking up in a meeting or attending a social gathering—feel unbearable. Over time, social anxiety can severely limit relationships, education, and career opportunities.
Specific Phobias involve intense fear of particular objects or situations, such as heights, flying, spiders, or needles. While many people have mild fears, phobias are extreme and lead to avoidance that interferes with normal life. The fear is often recognized as irrational, yet still feels impossible to control.
These categories help clinicians diagnose and treat anxiety disorders more effectively, but they often overlap. Someone might experience symptoms from more than one type, and that’s completely normal. Anxiety doesn’t like neat boxes—it tends to spill over into different areas of life.
Generalized Anxiety Disorder Explained in Detail
Generalized Anxiety Disorder (GAD) is one of the most pervasive anxiety disorders, affecting millions worldwide. Unlike other anxiety disorders that are triggered by specific situations or objects, GAD is characterized by a persistent, all-encompassing sense of worry. People with GAD often feel as though they are constantly on edge, unable to turn off the internal dialogue of “what if” scenarios.
Daily life with GAD can feel like trying to carry a backpack full of bricks that only gets heavier over time. Ordinary responsibilities—paying bills, managing work tasks, or even planning social events—become monumental challenges. Sleep often suffers, as racing thoughts keep the mind alert even when the body is exhausted. Physical symptoms such as headaches, muscle tension, digestive issues, and fatigue are common, and the cycle of worry and physical discomfort reinforces itself over time.
Triggers for GAD can be both internal and external. Stressful life events, health concerns, financial problems, and interpersonal conflicts can intensify anxiety. Interestingly, even positive events, like getting married or moving to a new home, can trigger worry for someone with GAD. This is because the underlying issue is not the events themselves but the brain’s heightened sensitivity to perceived threats.
People with GAD often struggle with concentration and decision-making. Their mind becomes so occupied with worst-case scenarios that focusing on the present moment feels impossible. Socially, individuals may appear tense or irritable, and they might avoid sharing their anxieties to prevent judgment or burdening others.
Treatment is highly effective when tailored to the individual. Cognitive Behavioral Therapy (CBT) can help identify patterns of catastrophic thinking and develop strategies to manage worry. Medications, such as selective serotonin reuptake inhibitors (SSRIs), can help stabilize mood and reduce excessive anxiety. Lifestyle changes, including regular exercise, mindfulness practices, and proper sleep hygiene, play an essential role in managing GAD long-term.
Understanding GAD requires empathy. It’s not simply about “thinking positively” or “relaxing.” For someone living with GAD, anxiety is a constant, unwelcome companion. Recognizing its impact and taking proactive steps toward treatment can significantly improve quality of life.
Panic Disorder and Panic Attacks
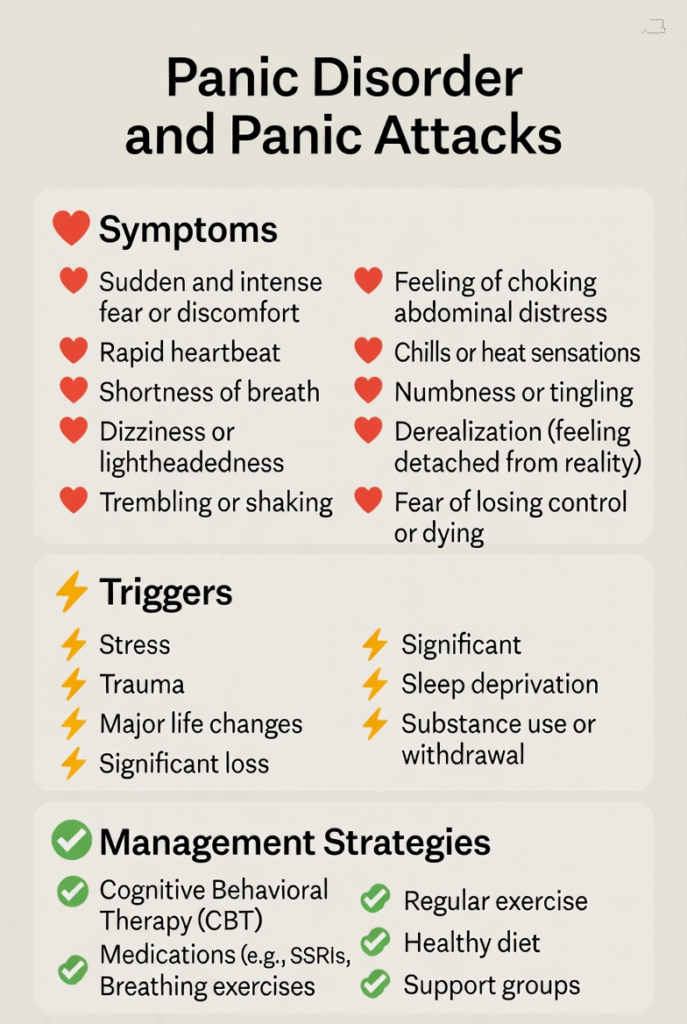
Panic disorder is another anxiety condition that can be intensely disruptive. Its hallmark is the panic attack—a sudden, overwhelming surge of fear and physical symptoms that can leave individuals feeling as though they are in immediate danger. The scary part? Panic attacks often strike out of nowhere, without an obvious trigger, making them unpredictable and frightening.
During a panic attack, the body’s “fight or flight” response goes into overdrive. Heart rate spikes, breathing becomes rapid or shallow, dizziness sets in, and chest pain or tightness may occur. Many people feel like they are having a heart attack or about to pass out. These attacks usually peak within 10 minutes but can leave lingering fear and exhaustion for hours afterward.
Panic disorder develops when individuals begin to fear having additional panic attacks. This fear often leads to avoidance behaviors, where people might skip certain places, activities, or even leave their home entirely to reduce the risk of an attack. Over time, this avoidance can evolve into agoraphobia—a fear of situations where escape might be difficult.
The causes of panic disorder are multifaceted. Genetics, brain chemistry, stressful life events, and certain personality traits can all contribute. Studies have shown that overactivity in the amygdala, coupled with hypersensitivity to stress hormones, plays a central role in the sudden surge of panic.
Treatment for panic disorder usually combines psychotherapy and medication. CBT focuses on teaching individuals to recognize the signs of an impending panic attack, challenge catastrophic thoughts, and gradually confront feared situations. Medications, including SSRIs, SNRIs, or benzodiazepines, may reduce attack frequency and intensity. Relaxation techniques, mindfulness, and controlled breathing exercises are often recommended as complementary tools.
Living with panic disorder can feel isolating, but understanding the condition helps normalize the experience and empowers individuals to regain control.
Social Anxiety Disorder: Fear of Being Seen

Social Anxiety Disorder (SAD) is not just shyness. It’s an intense, persistent fear of being judged, embarrassed, or scrutinized in social situations. While almost everyone feels self-conscious at times, people with SAD experience extreme anxiety that can interfere with work, school, relationships, and everyday activities.
Social anxiety often begins in childhood or adolescence, sometimes triggered by negative social experiences, bullying, or overcritical parenting. The brain becomes hyper-aware of potential judgment, scanning every facial expression, tone of voice, or glance for signs of disapproval. This heightened vigilance can feel exhausting, leaving individuals preoccupied with self-monitoring rather than engaging naturally.
Symptoms include excessive worry before social events, physical reactions like sweating, trembling, nausea, or blushing, and behavioral changes such as avoiding social gatherings, public speaking, or even eating in front of others. Over time, avoidance behaviors reinforce anxiety, creating a cycle that is hard to break without intervention.
Treatment for social anxiety often involves exposure therapy, a form of CBT where individuals gradually face feared social situations in a controlled and supportive way. Social skills training and mindfulness-based interventions can also improve confidence and reduce stress. Medications like SSRIs or SNRIs may help alleviate intense symptoms, making therapy more manageable.
Despite its challenges, many people with social anxiety lead successful and fulfilling lives. The key is recognizing the disorder early and developing coping strategies, support systems, and treatment plans that foster gradual, sustainable improvement.
Specific Phobias and Irrational Fears
Specific phobias involve intense, irrational fear of particular objects, animals, or situations. Common phobias include heights, flying, spiders, injections, or confined spaces. The fear is disproportionate to the actual threat and often triggers immediate avoidance behavior.
Phobias develop through a combination of genetics, brain wiring, and life experiences. A traumatic experience—such as a fall from a height or a severe allergic reaction—can create lasting fear. Once a phobia takes root, avoidance reinforces it. The more someone avoids the feared object or situation, the stronger the fear becomes.
Symptoms are both emotional and physical. Emotional symptoms include overwhelming dread, panic, or a sense of impending doom when confronted with the phobic object. Physical symptoms mirror other anxiety disorders: rapid heartbeat, sweating, shaking, nausea, and even difficulty breathing.
Treatment is highly effective. Exposure therapy gradually introduces the person to the feared object or situation in a safe and controlled manner, helping the brain learn that the threat is not as dangerous as perceived. Cognitive strategies, relaxation techniques, and support from therapists can further accelerate progress.
While phobias may seem irrational to others, they are very real to those experiencing them. Understanding and compassion are key to supporting someone facing these fears.
Symptoms of Anxiety Disorders
Anxiety disorders manifest in various ways, affecting the mind, body, and behavior. Recognizing the signs is essential for early intervention and treatment. While symptoms vary depending on the type of anxiety disorder, there are common patterns worth noting.
Emotional Symptoms: These include persistent worry, fear, or dread that feels uncontrollable. People often describe feeling “on edge” or tense. Irritability is common, and even minor challenges can trigger intense stress. Anxiety can also create feelings of restlessness, helplessness, or doom, making it difficult to enjoy life or feel at peace.
Physical Symptoms: Anxiety is as much a physical experience as a mental one. Muscle tension, headaches, and stomach issues are common. Some people experience palpitations, rapid breathing, sweating, dizziness, or even tingling sensations. Sleep disturbances, including difficulty falling asleep or waking frequently at night, are frequent complaints. Chronic anxiety can also contribute to fatigue, lowered immunity, and other health complications.
Behavioral Symptoms: Avoidance is a hallmark of anxiety disorders. Individuals may skip social events, delay tasks, or avoid situations that provoke stress. Compulsive behaviors, such as repetitive checking or reassurance-seeking, can develop, particularly in obsessive-compulsive-related anxiety. Performance anxiety can impact school, work, or sports, creating a pattern of missed opportunities and self-doubt.
It’s important to understand that anxiety symptoms are not a sign of weakness—they are the body and mind’s response to perceived threats, real or imagined. The severity of symptoms varies among individuals and may fluctuate over time. Recognizing them early and seeking help can prevent escalation and improve quality of life.
Causes and Risk Factors of Anxiety Disorders
Anxiety disorders do not have a single cause. Instead, they arise from a complex interplay of biological, psychological, and environmental factors. Understanding these causes can help reduce stigma and guide effective treatment.
Trauma and Stress: Exposure to traumatic events—such as abuse, accidents, natural disasters, or loss of a loved one—can trigger long-lasting anxiety. Chronic stress, whether from work, finances, or relationships, can also make the brain more sensitive to anxiety.
Personality Traits: Certain personality traits, like perfectionism, sensitivity, or a tendency toward negative thinking, increase vulnerability to anxiety disorders. People who are naturally cautious or highly self-critical may be more prone to excessive worry.
Genetics: Family history plays a significant role. If a close relative has an anxiety disorder, the likelihood of developing one is higher. Genetics may influence brain chemistry, stress response, and temperament.
Brain Chemistry: Neurotransmitters such as serotonin, GABA, and norepinephrine regulate mood and anxiety. Imbalances in these chemicals can disrupt the brain’s ability to manage stress, contributing to anxiety disorders.
Lifestyle Influences: Poor sleep, excessive caffeine or alcohol, lack of physical activity, and unhealthy diets can exacerbate anxiety. Conversely, healthy routines can reduce symptoms and enhance resilience.
Understanding these risk factors is crucial for prevention and intervention. Anxiety disorders are not a personal failing—they are influenced by biological and environmental factors, often beyond conscious control.
How Anxiety Disorders Are Diagnosed
Diagnosing anxiety disorders involves a thorough evaluation by a mental health professional. There is no single test for anxiety; instead, diagnosis relies on clinical assessment and observation.
Clinical Assessments: A psychologist, psychiatrist, or primary care physician will review symptoms, duration, and severity. They may ask about family history, medical conditions, lifestyle, and recent stressors. This helps differentiate between normal stress and a diagnosable disorder.
Self-Report Tools: Standardized questionnaires, like the Generalized Anxiety Disorder-7 (GAD-7) or the Social Phobia Inventory (SPIN), help quantify symptom severity. These tools provide a structured way for patients to describe their experiences.
Interviews: Clinicians often conduct detailed interviews to explore emotional, cognitive, and behavioral patterns. They may inquire about triggers, coping strategies, and the impact of symptoms on daily life.
Accurate diagnosis is critical because treatment varies depending on the specific type of anxiety disorder. Early recognition allows for timely intervention, which can prevent symptoms from worsening and improve overall quality of life.
Treatment Options for Anxiety Disorders
Anxiety disorders are highly treatable, and effective strategies typically combine therapy, medication, and lifestyle adjustments. Treatment plans are tailored to the individual, taking into account severity, personal preferences, and underlying causes.
Psychotherapy: Cognitive Behavioral Therapy (CBT) is the most widely used approach. It helps individuals identify negative thought patterns, challenge irrational fears, and develop practical coping strategies. Exposure therapy, a CBT technique, gradually confronts feared situations to reduce avoidance.
Medication: Depending on the type and severity of the disorder, medications such as SSRIs, SNRIs, or benzodiazepines may be prescribed. These help regulate neurotransmitters, reduce excessive worry, and prevent panic attacks.
Combination Approaches: Often, combining therapy and medication yields the best results. Psychotherapy addresses root causes and coping strategies, while medication provides relief from overwhelming symptoms.
Alternative and Complementary Strategies: Mindfulness meditation, yoga, breathing exercises, and other relaxation techniques can help manage anxiety in daily life. Support groups and peer networks also provide emotional support and shared coping strategies.
The key to effective treatment is consistency. Anxiety disorders are chronic conditions, but with the right interventions, symptoms can be significantly reduced, allowing individuals to reclaim control over their lives.
Cognitive Behavioral Therapy (CBT) and Anxiety
Cognitive Behavioral Therapy (CBT) is widely considered the gold standard for anxiety treatment. Its effectiveness lies in its structured approach, combining cognitive restructuring with behavioral exercises.
CBT works by identifying distorted or unhelpful thoughts and replacing them with more realistic, constructive ones. For instance, a person with social anxiety may believe, “Everyone is judging me.” CBT challenges this thought, asking for evidence and encouraging gradual exposure to social interactions.
Behavioral strategies include exposure exercises, relaxation techniques, and skills training. Over time, these strategies reduce avoidance, increase confidence, and retrain the brain’s response to fear.
CBT is practical, goal-oriented, and often time-limited, making it appealing to many patients. Research consistently shows CBT’s long-term effectiveness, with benefits that persist even after therapy ends. When combined with medication, CBT can significantly improve outcomes for severe anxiety disorders.
Medications Used to Treat Anxiety Disorders
Medications can be a crucial part of managing anxiety disorders, particularly for moderate to severe cases where symptoms significantly impact daily life. While therapy addresses thought patterns and coping strategies, medications target the brain’s chemical balance to reduce physiological and emotional distress.
SSRIs (Selective Serotonin Reuptake Inhibitors): SSRIs, such as sertraline, fluoxetine, and escitalopram, are commonly prescribed for anxiety disorders. They work by increasing serotonin levels in the brain, which helps stabilize mood and reduce excessive worry. SSRIs are usually well-tolerated but may take several weeks to show full benefits.
SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors): SNRIs, including venlafaxine and duloxetine, target both serotonin and norepinephrine. They can be particularly helpful for generalized anxiety disorder and panic disorder. Side effects are similar to SSRIs and may include nausea, dizziness, or sleep disturbances.
Benzodiazepines: Drugs like diazepam and lorazepam act quickly to calm the nervous system, making them effective for acute anxiety or panic attacks. However, they are generally prescribed short-term due to the risk of dependency and tolerance. Long-term use requires careful monitoring by a physician.
Other Medications: Certain antihistamines, beta-blockers, or anticonvulsants may be used off-label to manage specific anxiety symptoms. Beta-blockers, for example, can reduce physical symptoms such as racing heart or tremors during performance anxiety.
While medication can be life-changing, it’s most effective when combined with therapy and lifestyle adjustments. Each individual responds differently, so finding the right medication and dosage often requires patience and collaboration with a healthcare provider.
Lifestyle Changes That Help Manage Anxiety
Lifestyle adjustments play a vital role in managing anxiety disorders. Small, consistent changes can complement therapy and medication, helping reduce symptoms and increase resilience.
Sleep: Poor sleep amplifies anxiety. Establishing a regular sleep schedule, avoiding screens before bed, and creating a calm bedtime routine can dramatically improve emotional regulation.
Exercise: Physical activity releases endorphins and reduces stress hormones like cortisol. Even moderate exercise, such as walking, swimming, or yoga, can decrease anxiety and improve mood.
Nutrition: A balanced diet rich in whole foods, lean protein, fruits, and vegetables supports brain health. Limiting caffeine, alcohol, and processed sugar can prevent spikes in anxiety and jitteriness.
Mindfulness and Meditation: Mindfulness practices encourage focusing on the present moment, reducing the tendency to ruminate on past events or worry about the future. Techniques like deep breathing, progressive muscle relaxation, and guided meditation are highly effective.
Stress Management: Identifying stress triggers and creating coping strategies, such as journaling, art, or hobbies, helps manage anxiety proactively rather than reactively.
Integrating these lifestyle changes into daily routines creates a foundation for mental well-being. While they may not eliminate anxiety entirely, they reduce its intensity and improve overall quality of life.
Living With Anxiety Disorders
Living with an anxiety disorder can feel like walking through life with a constant shadow, but it is possible to lead a fulfilling, meaningful life. The key is developing coping strategies, self-compassion, and resilience.
Coping Strategies: Techniques such as grounding exercises, mindfulness, structured routines, and exposure therapy can help manage anxiety in real-time. Preparing for anxiety triggers in advance can reduce the feeling of helplessness.
Support Systems: Talking openly with friends, family, or support groups provides validation and encouragement. Feeling understood reduces isolation, which is often a major source of stress for individuals with anxiety.
Self-Compassion: Anxiety is not a character flaw. Treating oneself with patience and kindness, rather than harsh judgment, improves recovery outcomes and emotional resilience.
Setting Realistic Goals: Breaking tasks into manageable steps prevents overwhelm and reinforces a sense of control. Celebrating small victories can counteract the negative self-talk common in anxiety disorders.
Over time, consistent practice of these strategies can reduce the frequency and severity of anxiety episodes. While living with anxiety is challenging, it is not a life sentence. Many people find that with the right support and tools, they thrive personally, professionally, and socially.
Anxiety Disorders in Children and Adolescents
Anxiety disorders are not limited to adults; children and teenagers can also experience these conditions, sometimes in ways that differ from adults. Early recognition is crucial to prevent long-term effects.
Early Signs: In children, anxiety may manifest as excessive worry about school performance, social interactions, or separation from parents. Physical complaints such as stomachaches or headaches are common. Adolescents may show irritability, sleep disturbances, or avoidance behaviors.
Impact if Untreated: Untreated anxiety in youth can affect academic performance, social development, and self-esteem. It may also increase the risk of depression, substance abuse, or ongoing anxiety into adulthood.
Treatment Approaches: Cognitive-behavioral therapy adapted for children, family therapy, and, in some cases, medication, are effective. Teaching coping skills early helps children develop resilience and prevents anxiety from becoming a lifelong burden.
Supporting children with anxiety involves patience, understanding, and collaboration with schools and healthcare providers. Early intervention often results in better outcomes and empowers children to navigate life confidently.
When to Seek Professional Help
Recognizing when to seek professional help is critical. While occasional anxiety is normal, persistent or intense anxiety that interferes with daily life warrants attention.
Warning Signs:
- Constant worry or dread that doesn’t go away
- Panic attacks or physical symptoms such as chest pain or shortness of breath
- Avoidance of social situations or responsibilities
- Sleep disturbances or extreme fatigue
- Difficulty concentrating or making decisions
Breaking the Stigma: Many people hesitate to seek help due to shame or fear of being judged. It’s important to remember that anxiety disorders are medical conditions, not personal weaknesses. Seeking professional guidance is a courageous and proactive step toward well-being.
Therapists, psychiatrists, psychologists, and primary care physicians can provide assessment, treatment plans, and ongoing support. Early intervention improves outcomes and can significantly reduce the impact of anxiety disorders on daily life.
The Future of Anxiety Disorder Treatment
The treatment landscape for anxiety disorders is evolving, with innovative approaches expanding access and effectiveness.
Digital Therapy: Teletherapy and mental health apps make therapy accessible to more people. Guided online CBT programs, virtual support groups, and mindfulness apps provide convenient tools for managing anxiety.
Emerging Research: Scientists are exploring novel treatments, including neurofeedback, transcranial magnetic stimulation (TMS), and new medications targeting specific brain pathways. Understanding the genetics and neuroscience of anxiety may lead to more personalized and effective interventions in the future.
Integration of Mind-Body Approaches: Combining traditional therapy with mindfulness, yoga, biofeedback, and lifestyle interventions is gaining traction as an evidence-based approach to holistic anxiety management.
With these advancements, the future looks promising. Anxiety disorders will remain challenging, but innovations in science, technology, and therapy continue to improve quality of life for millions.
Real-Life Experiences of Living With Anxiety Disorders
Imagine waking up in the morning, and before your feet even touch the floor, your mind is racing. You’re worried about things that haven’t even happened yet: “What if I mess up at work today?” or “What if something happens to my loved ones?” This is a daily reality for millions of people with anxiety disorders. Anxiety doesn’t just disappear after a cup of coffee or a pep talk—it’s persistent, relentless, and can feel like an invisible weight that never leaves.
Take Sarah, for example, a 29-year-old software developer. On the outside, she appears calm and organized, but internally, she struggles with generalized anxiety disorder. Even small emails or harmless text messages trigger overthinking. Is this urgent? Did I say the wrong thing? Will my boss be upset? At night, her mind refuses to switch off, leaving her tossing and turning for hours. This is the subtle yet exhausting nature of anxiety disorders: they are not always visible, but they shape daily life profoundly.
Panic disorder adds a different layer of challenge. John, a 35-year-old teacher, experienced his first panic attack during a parent-teacher conference. Suddenly, his heart raced, his chest felt tight, and he feared he might collapse in front of everyone. Even though there was no actual danger, his brain reacted as if he were in mortal peril. After this first attack, John began avoiding school events, afraid another attack would occur. Over time, this avoidance became isolating, affecting both his career and personal life.
Social anxiety disorders can also quietly steal opportunities. Emily, a university student, avoided participating in class discussions and social events because she feared being judged. Over time, she missed chances for networking, forming friendships, and building confidence. Even everyday interactions like ordering coffee or talking to a neighbor caused intense stress. But with therapy and gradual exposure exercises, she learned that facing her fears step by step allowed her to reclaim parts of life she had been avoiding.
Coping Strategies That Actually Work
It’s one thing to read about CBT, medications, or mindfulness in a textbook—it’s another to see them applied in real life. Coping strategies for anxiety disorders work best when they are practical, consistent, and personalized.
- Grounding Techniques: These involve bringing your mind back to the present. For example, during a panic attack, noticing five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste can quickly reduce anxiety’s intensity.
- Daily Journaling: Writing down worries can help separate irrational thoughts from real concerns. Seeing your anxiety on paper often reduces its power.
- Structured Routines: Establishing a predictable daily schedule provides a sense of control. Even simple tasks, like morning stretches, planning meals, or scheduling short breaks, can reduce anxiety’s grip.
- Exposure Practice: Gradually confronting feared situations—like attending a social event for five minutes and increasing over time—helps rewire the brain to respond more calmly.
- Mindfulness and Meditation: Apps like Headspace or Calm guide you through short sessions that focus on breathing and awareness. Even five minutes a day can reduce cortisol levels and improve emotional regulation over time.
The Role of Support Networks
Anxiety disorders are easier to manage when you have a supportive environment. Friends, family, mentors, and peers play a crucial role in helping individuals feel understood and less isolated.
- Open Communication: Talking openly about your anxiety with someone you trust reduces the burden of carrying it alone.
- Peer Support Groups: Sharing experiences with people who face similar struggles normalizes the experience and provides practical strategies.
- Professional Guidance: Therapists, counselors, and psychiatrists offer tools tailored to individual needs. Their role is not only to treat symptoms but also to teach sustainable coping strategies.
Preventing Anxiety From Taking Over Your Life
While anxiety disorders cannot always be completely prevented, proactive measures can reduce severity and prevent escalation:
- Early Intervention: Recognizing symptoms early—such as persistent worry, avoidance, or panic attacks—and seeking help can prevent long-term challenges.
- Healthy Lifestyle Choices: Exercise, nutrition, proper sleep, and mindfulness practices create a strong foundation for mental resilience.
- Stress Management Skills: Learning to manage deadlines, responsibilities, and interpersonal conflicts prevents chronic stress from triggering anxiety.
- Self-Compassion: Accepting that anxiety is a medical condition, not a personal failure, reduces guilt and fosters empowerment.
Conclusion
Anxiety disorders are complex, multifaceted conditions that touch millions of lives worldwide. They are not a sign of weakness but the result of intricate interactions between brain chemistry, genetics, environment, and life experiences. From generalized anxiety to social phobias and panic disorder, each condition presents unique challenges—but also opportunities for effective management and recovery.
Treatment combines therapy, medication, lifestyle adjustments, and support systems to reduce symptoms and improve daily functioning. Early recognition, understanding, and compassionate care are essential to breaking cycles of worry, fear, and avoidance. While living with anxiety is demanding, with the right tools and support, individuals can thrive personally, socially, and professionally.
The key takeaway is hope: anxiety disorders are treatable, manageable, and do not define a person’s worth or potential. Awareness, education, and proactive care empower individuals to regain control and live fulfilling lives.
Frequently Asked Questions (FAQs)
1. Can anxiety disorders be cured completely?
While anxiety disorders may not always be “cured” in the traditional sense, symptoms can be effectively managed through therapy, medication, and lifestyle strategies. Many people achieve long-term relief and lead full lives.
2. How long does it take for treatment to work?
The timeline varies. Therapy often shows noticeable improvements within 6–12 weeks, while medications may take 4–6 weeks for full effect. Consistency and combining approaches usually yield the best results.
3. Is anxiety hereditary?
Genetics play a role, increasing vulnerability, but anxiety is influenced by environmental and life factors as well. Having a family member with anxiety doesn’t guarantee you will develop it.
4. Are lifestyle changes really effective for managing anxiety?
Yes. Sleep, exercise, nutrition, stress management, and mindfulness practices significantly reduce symptoms and complement therapy and medication.
5. Can children experience anxiety disorders too?
Absolutely. Children and adolescents can develop anxiety disorders, often presenting differently than adults. Early intervention with therapy and coping strategies can prevent long-term challenges.