Introduction to Mental Disorders
Mental disorders are far more common than many people realize, yet they remain one of the most misunderstood aspects of human health. At their core, mental disorders are conditions that significantly affect how a person thinks, feels, behaves, or interacts with others. Just like physical illnesses, they can range from mild and temporary to severe and long-lasting. The difference is that mental disorders impact the mind, emotions, and behavior, often in ways that are invisible to the outside world. That invisibility is one of the main reasons why mental health issues are often ignored, minimized, or misunderstood.
In today’s fast-paced, always-connected world, mental health challenges are on the rise. Constant pressure to succeed, financial stress, social media comparison, isolation, and global uncertainty all play a role in shaping mental well-being. Mental disorders do not discriminate—they can affect anyone regardless of age, gender, culture, or socioeconomic status. From anxiety and depression to schizophrenia and bipolar disorder, these conditions touch millions of lives every single day.
Understanding mental disorders is the first step toward compassion, effective treatment, and prevention. When people are informed, they are more likely to recognize symptoms early, seek professional help, and support others without judgment. This guide is designed to break down complex concepts into simple, human terms, helping readers understand what mental disorders are, why they happen, and how they can be managed. Think of it as a roadmap—one that leads away from stigma and fear and toward awareness, empathy, and healing.
Understanding Mental Health vs. Mental Illness
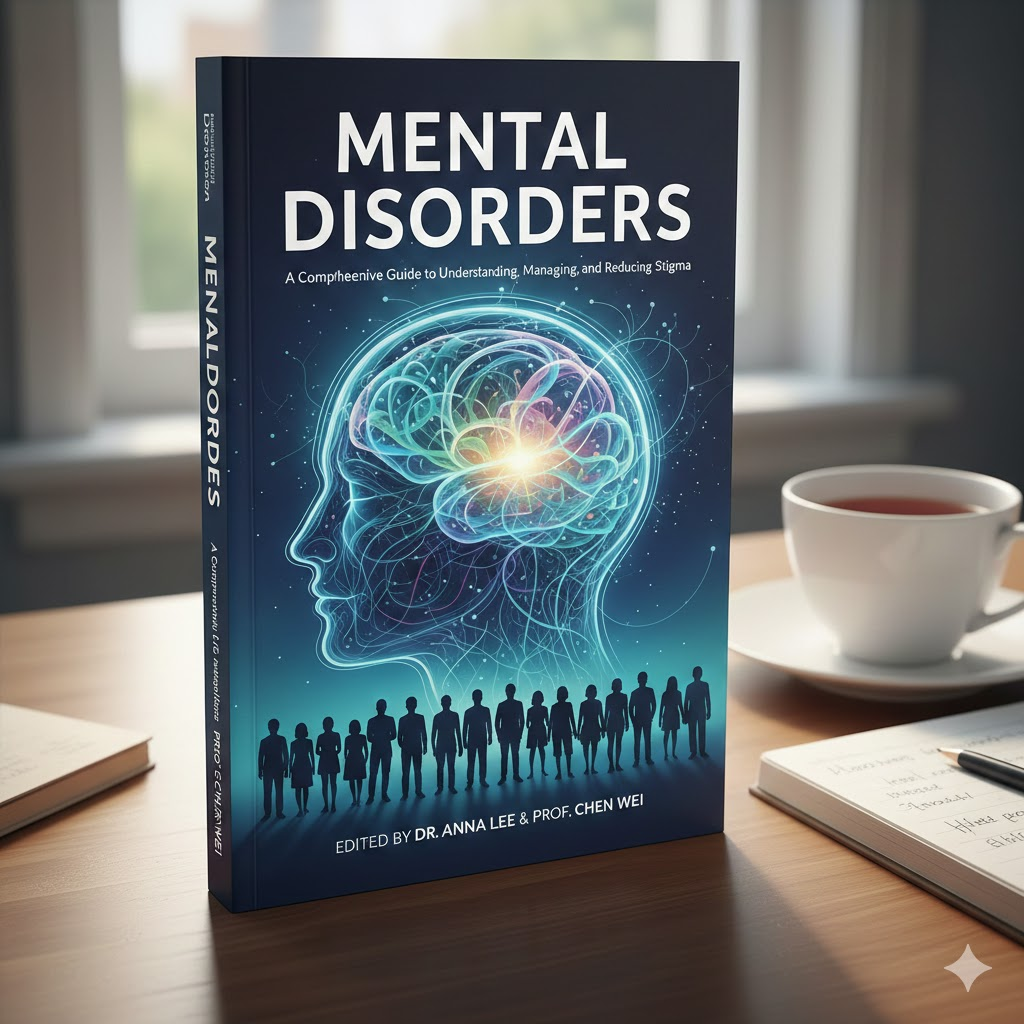
Mental health and mental illness are often used interchangeably, but they are not the same thing. Mental health refers to a person’s overall emotional, psychological, and social well-being. It influences how we handle stress, relate to others, make decisions, and cope with life’s ups and downs. Good mental health does not mean feeling happy all the time; it means being able to manage emotions, adapt to change, and recover from challenges.
Mental illness, on the other hand, refers to diagnosed conditions that disrupt a person’s thinking, mood, or behavior to a degree that interferes with daily functioning. Someone can experience poor mental health without having a diagnosable mental disorder, just as someone with a mental disorder can experience periods of stability and well-being. The relationship between mental health and mental illness is not black and white—it exists on a spectrum.
Imagine mental health as physical fitness. You don’t have to be an athlete to be healthy, and having a physical illness doesn’t define your overall worth or capabilities. In the same way, having a mental disorder does not define a person. It simply means they may need support, treatment, and understanding—just like anyone dealing with a physical condition.
Recognizing this distinction helps reduce stigma. When society views mental illness as a normal part of human health rather than a personal weakness, people feel safer seeking help. Open conversations about mental health encourage prevention, early intervention, and long-term recovery.
Common Types of Mental Disorders

Mental disorders come in many forms, each with its own symptoms, challenges, and treatment approaches. Understanding the most common categories can make these conditions feel less overwhelming and more approachable.
Anxiety Disorders
Anxiety disorders are among the most prevalent mental health conditions worldwide. While occasional anxiety is a normal response to stress, anxiety disorders involve excessive fear or worry that does not go away and often worsens over time. Generalized anxiety disorder is characterized by constant, uncontrollable worry about everyday matters. Panic disorder involves sudden, intense episodes of fear known as panic attacks, often accompanied by physical symptoms like a racing heart or shortness of breath. Social anxiety disorder causes extreme fear of social situations, leading many individuals to avoid interactions altogether.
Mood Disorders
Mood disorders primarily affect a person’s emotional state. Depression is one of the most common mental disorders, marked by persistent sadness, loss of interest, fatigue, and feelings of hopelessness. Bipolar disorder involves extreme mood swings, ranging from depressive lows to manic or hypomanic highs. These shifts can disrupt relationships, work, and daily routines if left untreated.
Psychotic Disorders
Psychotic disorders, such as schizophrenia, affect how a person perceives reality. Symptoms may include hallucinations, delusions, disorganized thinking, and difficulty distinguishing what is real from what is not. Although these conditions are often portrayed inaccurately in media, many individuals with psychotic disorders can lead fulfilling lives with proper treatment and support.
Personality, Eating, and Neurodevelopmental Disorders
Personality disorders involve enduring patterns of behavior and thinking that deviate from cultural expectations and cause distress. Eating disorders, such as anorexia nervosa and bulimia, are serious conditions related to food, body image, and self-esteem. Neurodevelopmental disorders, including autism spectrum disorder and ADHD, typically begin in childhood and affect learning, behavior, and social interaction.
Understanding these categories helps normalize mental disorders and highlights the importance of tailored treatment approaches.
Causes and Risk Factors of Mental Disorders
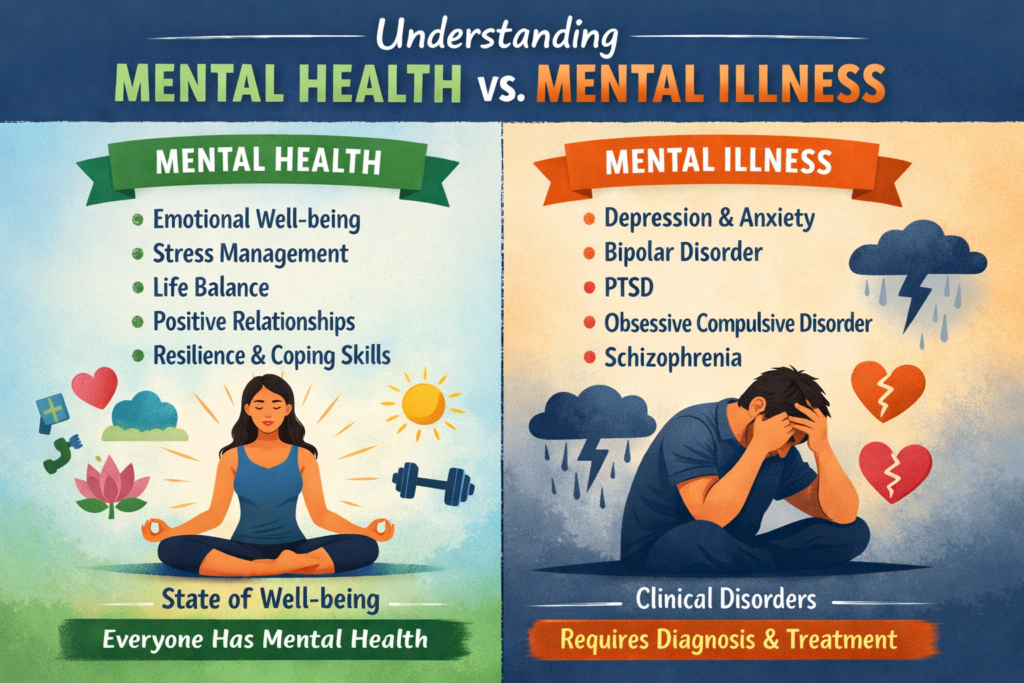
Mental disorders rarely have a single cause. Instead, they usually develop from a complex interaction of biological, psychological, and social factors. Understanding these causes helps remove blame and replaces it with clarity and compassion. Mental illness is not a personal failure or a lack of willpower; it is often the result of forces beyond an individual’s control.
Biological factors play a major role in many mental disorders. Genetics can increase vulnerability, meaning a person may inherit a higher risk if close family members have experienced mental health conditions. Brain chemistry is another key element. Neurotransmitters such as serotonin, dopamine, and norepinephrine help regulate mood, emotions, and behavior. When these chemicals are imbalanced, mental disorders like depression, anxiety, or schizophrenia may develop. Additionally, brain injuries, chronic illnesses, and hormonal changes can also contribute to mental health challenges.
Psychological factors include personality traits, coping mechanisms, and past experiences. Childhood trauma, abuse, neglect, or prolonged exposure to stress can significantly increase the risk of developing mental disorders later in life. People who struggle with low self-esteem, perfectionism, or difficulty managing emotions may also be more susceptible. Unresolved grief or major life transitions—such as divorce, loss of a loved one, or sudden change—can act as triggers.
Social and environmental factors are equally influential. Poverty, unemployment, discrimination, social isolation, and lack of access to healthcare all increase mental health risks. Living in a high-stress environment, experiencing bullying, or being exposed to violence can leave long-lasting psychological scars. Even cultural stigma around mental health can worsen symptoms by discouraging people from seeking help.
When these factors overlap, the risk becomes greater. Recognizing this layered reality helps shift the conversation from “What’s wrong with you?” to “What happened to you?”—a far more humane and productive approach.
Early Signs and Symptoms of Mental Disorders

Early detection of mental disorders can make a life-changing difference. The sooner symptoms are recognized, the sooner treatment and support can begin. However, early signs are often subtle and easy to dismiss, especially because they can resemble everyday stress or temporary emotional struggles.
Emotional symptoms are often the first indicators. These may include persistent sadness, excessive worry, intense fear, mood swings, irritability, or feelings of emptiness. A person might feel overwhelmed by emotions that seem out of proportion to the situation or struggle to feel joy in activities they once enjoyed. Emotional numbness can be just as concerning as emotional overload.
Behavioral symptoms can signal that something deeper is going on. These include withdrawing from friends and family, avoiding responsibilities, changes in sleep or appetite, increased substance use, or difficulty concentrating. Someone may appear unusually restless, aggressive, or detached. In severe cases, self-harm or suicidal thoughts may emerge, which always require immediate professional attention.
Physical symptoms are often overlooked but closely connected to mental health. Chronic headaches, stomach problems, fatigue, unexplained aches, or changes in weight can all be linked to mental disorders. The mind and body are deeply connected, and psychological distress frequently manifests physically.
Recognizing these signs does not mean jumping to conclusions, but it does mean paying attention. When symptoms persist for weeks or interfere with daily life, seeking professional help is a proactive and empowering step.
Diagnosis and Assessment of Mental Disorders
Diagnosing mental disorders is a careful and structured process, not a quick judgment. Mental health professionals use a combination of clinical interviews, standardized assessments, and diagnostic criteria to understand what a person is experiencing. The goal is accuracy, not labeling.
A clinical evaluation typically involves discussing symptoms, personal history, family history, and current life circumstances. Mental health professionals ask detailed questions to understand patterns, duration, and severity of symptoms. Honesty during this process is essential, as it helps ensure the most appropriate treatment plan.
Diagnostic criteria, such as those outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM), provide standardized guidelines for identifying specific conditions. These criteria help distinguish between similar disorders and ensure consistency across diagnoses. However, diagnosis is not just about checking boxes; it also involves professional judgment and individualized understanding.
Early diagnosis is critical. When mental disorders are identified early, treatment is often more effective, and long-term complications can be reduced. Early intervention can prevent symptoms from worsening and improve quality of life. Importantly, a diagnosis does not define a person—it simply provides a framework for understanding and healing.
Impact of Mental Disorders on Daily Life
Mental disorders can affect nearly every aspect of daily life, often in ways that outsiders cannot see. The impact is not limited to emotional distress; it extends into relationships, work, education, and physical health.
In relationships and family life, mental disorders can create misunderstandings and strain. Loved ones may struggle to understand mood changes, withdrawal, or unpredictable behavior. Communication can break down, leading to frustration on both sides. However, with education and support, families can become powerful allies in recovery.
In education and the workplace, mental disorders can interfere with concentration, motivation, and productivity. Students may struggle academically, while employees may face burnout, absenteeism, or reduced performance. Without supportive environments, individuals may feel ashamed or fear discrimination, which only worsens symptoms.
Physical health is also closely linked to mental well-being. Chronic stress, depression, and anxiety can weaken the immune system, increase the risk of heart disease, and worsen existing medical conditions. Conversely, poor physical health can negatively affect mental health, creating a cycle that is difficult to break.
Understanding these impacts highlights why mental health care is not optional—it is essential for overall well-being and societal health.
Mental Disorders and Stigma
Stigma remains one of the biggest barriers to mental health care. Despite increased awareness, many people still associate mental disorders with weakness, danger, or incompetence. These misconceptions are deeply harmful and often prevent individuals from seeking help.
Social stigma shows up in many forms, including discrimination, negative stereotypes, and dismissive language. People with mental disorders may be labeled as “lazy,” “unstable,” or “attention-seeking,” which minimizes their real struggles. Media portrayals often exaggerate or misrepresent mental illness, reinforcing fear and misunderstanding.
The effects of stigma can be devastating. Shame and fear of judgment may lead people to hide their symptoms, delay treatment, or isolate themselves. This silence can worsen mental health conditions and increase the risk of severe outcomes, including suicide.
Breaking the silence starts with open, honest conversations. Education, empathy, and inclusive language can challenge harmful beliefs. When people share their experiences and are met with understanding rather than judgment, stigma loses its power. Mental health is a human issue, and addressing it openly benefits everyone.
Treatment Options for Mental Disorders
Treatment for mental disorders is not one-size-fits-all. Effective care often involves a combination of approaches tailored to the individual’s needs, symptoms, and circumstances. The good news is that many mental disorders are highly treatable, and recovery is possible.
Psychotherapy, or talk therapy, helps individuals understand their thoughts, emotions, and behaviors. It provides tools for coping with stress, resolving conflicts, and changing unhelpful patterns. Therapy can be short-term or long-term, depending on the condition and personal goals.
Medication can be an important part of treatment, especially for moderate to severe mental disorders. Antidepressants, anti-anxiety medications, mood stabilizers, and antipsychotics help regulate brain chemistry. Medication is most effective when monitored by a qualified professional and combined with therapy.
Lifestyle and self-care strategies also play a crucial role. Regular exercise, balanced nutrition, quality sleep, mindfulness, and stress management can significantly improve mental well-being. While self-care alone is not a cure, it strengthens resilience and supports other treatments.
Role of Therapy in Mental Health Recovery
Therapy is often the cornerstone of mental health recovery. It provides a safe, supportive space where individuals can explore their experiences without fear of judgment. Different therapeutic approaches address different needs.
Cognitive behavioral therapy (CBT) focuses on identifying and changing negative thought patterns and behaviors. It is highly effective for anxiety, depression, and many other disorders. CBT helps individuals develop practical skills they can use in everyday life.
Psychodynamic therapy explores unconscious patterns, past experiences, and emotional conflicts that influence current behavior. This approach can lead to deep self-awareness and long-term change.
Group and family therapy emphasize connection and shared understanding. Group therapy reduces isolation by showing individuals they are not alone, while family therapy improves communication and support systems.
Medication and Psychiatric Care
Psychiatric medications are often misunderstood, yet they can be life-changing for many people. These medications help stabilize symptoms, making it easier to engage in therapy and daily activities.
Common types include antidepressants, anti-anxiety medications, mood stabilizers, and antipsychotics. Each works differently, and finding the right medication may take time. Professional guidance is essential to monitor effectiveness, adjust dosages, and manage side effects.
Medication does not change who a person is; it helps restore balance. When combined with therapy and support, psychiatric care can significantly improve quality of life.
Living with Mental Disorders
Living with a mental disorder is a journey, not a destination. While challenges may persist, many people learn to manage symptoms and build fulfilling lives.
Coping strategies such as journaling, mindfulness, setting boundaries, and maintaining routines can provide stability. Building resilience involves recognizing strengths, celebrating progress, and learning from setbacks.
Strong support systems—including friends, family, support groups, and professionals—make a profound difference. No one has to navigate mental health challenges alone.
Mental Disorders in Children and Adolescents
Mental disorders can begin early in life, making early intervention especially important. Conditions such as anxiety disorders, ADHD, depression, and autism spectrum disorder often appear in childhood or adolescence.
Parents and educators play a key role in recognizing changes in behavior, mood, or academic performance. Early support can prevent long-term difficulties and promote healthy development. Schools, families, and healthcare providers must work together to create supportive environments.
Mental Disorders in the Workplace
Mental health in the workplace is a growing concern. Stress, burnout, and untreated mental disorders affect productivity, morale, and employee retention.
Employers have a responsibility to create supportive work environments that prioritize well-being. Flexible schedules, mental health resources, and open communication reduce stigma and improve performance. When employees feel supported, everyone benefits.
Prevention and Mental Health Promotion
While not all mental disorders can be prevented, many risk factors can be reduced. Stress management, healthy routines, social connection, and access to care all promote mental well-being.
Community awareness and education empower people to seek help early and support one another. Prevention starts with understanding and compassion.
Future of Mental Health Care
The future of mental health care is evolving rapidly. Digital mental health solutions, such as teletherapy and mental health apps, are increasing access to care. Global initiatives and policy reforms are also placing mental health at the center of public health discussions.
Innovation, combined with empathy, holds the promise of a more inclusive and effective mental health system.
Conclusion
Mental disorders are a fundamental part of the human health experience, affecting millions of people across the globe. Understanding their causes, symptoms, and treatments helps replace fear with knowledge and stigma with compassion. With the right support, treatment, and awareness, individuals with mental disorders can lead meaningful, productive, and joyful lives. Mental health matters—and so does every person’s story.
Frequently Asked Questions
1. Are mental disorders permanent?
No, many mental disorders are treatable, and symptoms can be managed or significantly reduced with proper care.
2. Can mental disorders affect physical health?
Yes, mental and physical health are closely connected, and each can influence the other.
3. Is therapy effective without medication?
For some people, therapy alone is effective, while others benefit from a combination of therapy and medication.
4. How can I support someone with a mental disorder?
Listen without judgment, encourage professional help, and educate yourself about their condition.
5. When should someone seek help for mental health concerns?
When symptoms persist, worsen, or interfere with daily life, seeking professional help is recommended.