Introduction: Why Mental Illness Matters More Than Ever

Mental illness is not a distant problem that affects “other people.” It’s personal, close, and woven into the fabric of our everyday lives. Chances are, someone you love—or even you—has struggled with mental health at some point. In today’s fast-paced, hyper-connected world, stress, anxiety, depression, and emotional exhaustion have become almost normalized. But just because something is common doesn’t mean it should be ignored.
Mental illness affects how people think, feel, act, and cope with daily life. It influences relationships, careers, physical health, and self-worth. Yet, despite its widespread impact, mental illness is still misunderstood, stigmatized, and often pushed into the shadows. People suffer silently, afraid of being judged, labeled, or dismissed.
The truth is simple: mental illness is a health condition, just like diabetes or heart disease. It deserves compassion, proper care, and open conversation. When we understand mental illness better, we replace fear with knowledge and judgment with empathy. This article dives deep into what mental illness really is, why it happens, how it shows up, and—most importantly—how people can heal, manage, and live fulfilling lives despite it.
Let’s break the silence together and talk honestly about mental illness—because mental health is human health.
Understanding Mental Illness

Mental illness is a broad term that refers to conditions affecting a person’s mood, thinking, behavior, or emotional regulation. These conditions can be temporary or long-lasting, mild or severe, and they often interfere with daily functioning. Mental illness doesn’t define who a person is, but it does shape how they experience the world.
One of the biggest misunderstandings is confusing mental illness with weakness or a lack of willpower. That couldn’t be further from the truth. Mental illness arises from complex interactions between biological, psychological, and social factors. You can’t simply “snap out of it” any more than you can will away a broken bone.
It’s also important to understand the difference between mental health and mental illness. Mental health exists on a spectrum. Everyone has mental health, just like everyone has physical health. Mental illness occurs when mental health challenges become persistent, overwhelming, and disruptive to daily life.
Common myths suggest that people with mental illness are dangerous, incapable, or unreliable. In reality, most people with mental illness lead productive, meaningful lives, especially when they receive proper support. These misconceptions cause real harm by discouraging people from seeking help and reinforcing shame.
Understanding mental illness starts with education. When we replace assumptions with facts, we create space for empathy, support, and healing.
The Science Behind Mental Illness
Mental illness is deeply rooted in brain function and biology. The brain is an incredibly complex organ, responsible for emotions, memory, decision-making, and behavior. When its delicate balance is disrupted, mental health conditions can emerge.
Neurotransmitters—chemical messengers like serotonin, dopamine, and norepinephrine—play a major role in mental health. When these chemicals are imbalanced, mood disorders, anxiety, and other conditions can develop. For example, low serotonin levels are often linked to depression, while dopamine dysregulation is associated with schizophrenia.
Genetics also play a significant role. Mental illness can run in families, meaning some people are biologically more vulnerable. However, having a genetic predisposition doesn’t guarantee someone will develop a mental illness. Environment and life experiences often determine whether those genes are activated.
Environmental factors such as trauma, chronic stress, abuse, neglect, poverty, and social isolation can profoundly affect mental health. The brain is shaped by experiences, especially during childhood. Adverse experiences can alter brain development and stress responses, increasing the risk of mental illness later in life.
Mental illness is not caused by a single factor. It’s more like a puzzle, where biology, psychology, and environment fit together in unique ways for each individual.
Types of Mental Illness

Mental illness comes in many forms, each with its own patterns, challenges, and treatments. Understanding these categories helps reduce fear and promotes early recognition.
Anxiety disorders are among the most common mental health conditions. They include generalized anxiety disorder, panic disorder, social anxiety, and phobias. People with anxiety disorders experience excessive fear or worry that feels uncontrollable and overwhelming, often accompanied by physical symptoms like rapid heartbeat, sweating, and restlessness.
Mood disorders primarily affect emotional states. Depression causes persistent sadness, loss of interest, fatigue, and feelings of worthlessness. Bipolar disorder involves extreme mood swings, ranging from depressive lows to manic highs, affecting judgment, energy, and behavior.
Psychotic disorders, such as schizophrenia, impact a person’s perception of reality. Symptoms may include hallucinations, delusions, disorganized thinking, and emotional withdrawal. These conditions are often misunderstood and heavily stigmatized, yet they are treatable with proper care.
Personality disorders involve long-term patterns of behavior and inner experiences that differ significantly from cultural expectations. These patterns can affect relationships, self-image, and emotional regulation.
Trauma-related disorders, including post-traumatic stress disorder, develop after experiencing or witnessing traumatic events. They can cause flashbacks, nightmares, emotional numbness, and heightened alertness.
Each type of mental illness is unique, but all deserve understanding and compassion.
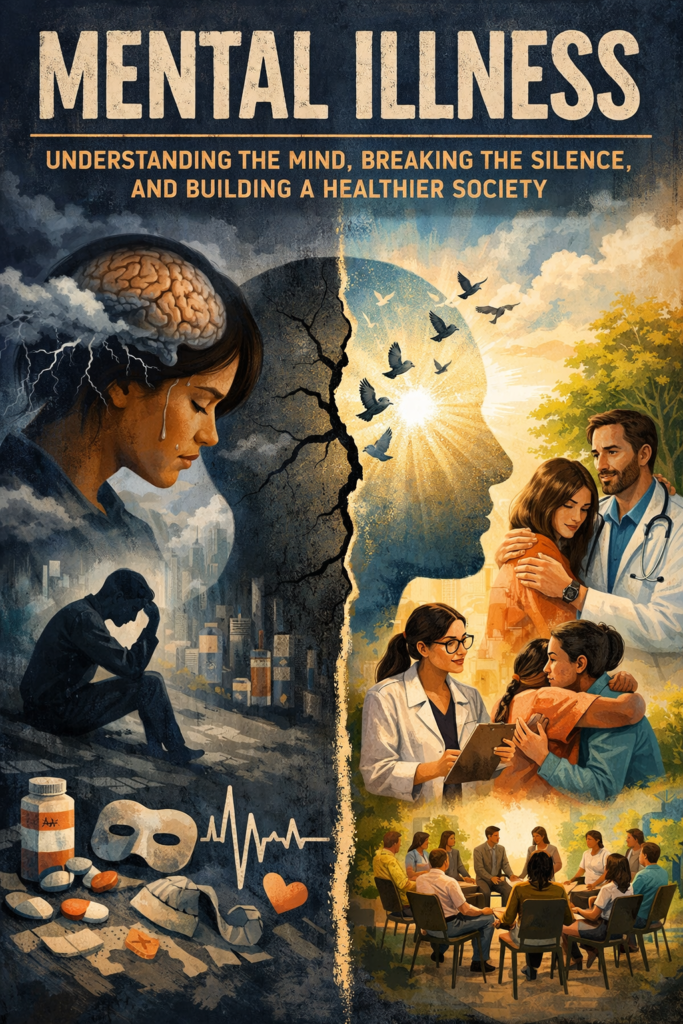
Signs and Symptoms of Mental Illness
Mental illness doesn’t always announce itself loudly. Sometimes, it creeps in quietly, disguised as stress, tiredness, or moodiness. Recognizing the signs early can make a huge difference in outcomes.
Emotional symptoms often include persistent sadness, fear, irritability, mood swings, or emotional numbness. People may feel overwhelmed by feelings they can’t explain or control.
Behavioral changes are another key indicator. These might include withdrawing from social activities, changes in sleep or appetite, difficulty concentrating, increased substance use, or neglecting responsibilities.
Physical symptoms are frequently overlooked. Headaches, stomach problems, chronic fatigue, and unexplained aches can all be linked to mental health conditions. The mind and body are deeply connected, and distress often shows up physically.
Symptoms become serious when they interfere with daily life, relationships, or safety. Thoughts of self-harm, suicide, or harming others require immediate professional attention. Ignoring these signs doesn’t make them go away—it often makes them worse.
Listening to your mind and body is not a weakness. It’s an act of self-respect.
Causes and Risk Factors
Mental illness rarely has a single cause. Instead, it develops through a combination of risk factors that interact over time.
Biological causes include genetics, brain chemistry, hormonal imbalances, and medical conditions. These factors can create vulnerability but don’t act alone.
Psychological factors such as personality traits, coping skills, self-esteem, and past trauma play a major role. People who struggle to process emotions or manage stress may be more susceptible.
Social and cultural influences are powerful. Poverty, discrimination, loneliness, violence, and lack of support can significantly increase the risk of mental illness. Humans are social beings, and isolation can be as damaging as physical illness.
Lifestyle factors like poor sleep, lack of exercise, unhealthy diet, and substance abuse can also contribute. These habits don’t cause mental illness on their own, but they can worsen symptoms and delay recovery.
Understanding causes helps shift blame away from individuals and toward a more compassionate, holistic view.
Mental Illness Across Different Life Stages
Mental illness can appear at any stage of life, but it often looks different depending on age and circumstances.
In childhood and adolescence, mental illness may show up as behavioral problems, academic struggles, or emotional outbursts. Conditions like ADHD, anxiety, and depression often begin early but go unnoticed or dismissed as “phases.”
In adulthood, responsibilities, relationships, and work pressures can intensify mental health challenges. Depression, anxiety, and substance use disorders are common during these years, especially when stress is chronic.
Aging brings its own mental health concerns. Loneliness, grief, cognitive decline, and physical illness can increase the risk of depression and anxiety in older adults. Mental health in later life is often overlooked, despite its importance.
Mental illness doesn’t discriminate by age. Awareness at every life stage is essential for early intervention and support.
Conclusion: Hope, Healing, and Humanity
Mental illness is not a flaw in character, a sign of weakness, or something to be hidden away in silence. It is a deeply human experience—one that touches thoughts, emotions, relationships, and daily life in ways both visible and unseen. When we step back and truly understand mental illness, we realize it is not about being broken; it is about being human in a world that can be overwhelming, demanding, and at times, unforgiving.
The most powerful shift happens when we replace judgment with curiosity and fear with compassion. Mental illness does not take away a person’s value, intelligence, creativity, or potential. With the right support, treatment, and understanding, people living with mental illness can heal, grow, and lead meaningful, fulfilling lives. Recovery is not always linear, and healing does not mean the absence of struggle—it means learning how to live well despite it.
As a society, we have a responsibility to talk openly, listen without interrupting, and support without conditions. Whether it’s seeking help for yourself, checking in on a loved one, or challenging harmful stereotypes, every small action matters. Mental health care should be accessible, conversations should be normalized, and no one should feel ashamed for needing help.
At the heart of it all is hope. Hope that awareness leads to acceptance. Hope that science continues to improve treatment. Hope that future generations grow up in a world where mental health is treated with the same urgency and respect as physical health. When we choose empathy over silence, we don’t just change individual lives—we create a healthier, more humane world for everyone.